Peripheral Arterial Disease: Symptoms, Causes And Treatment
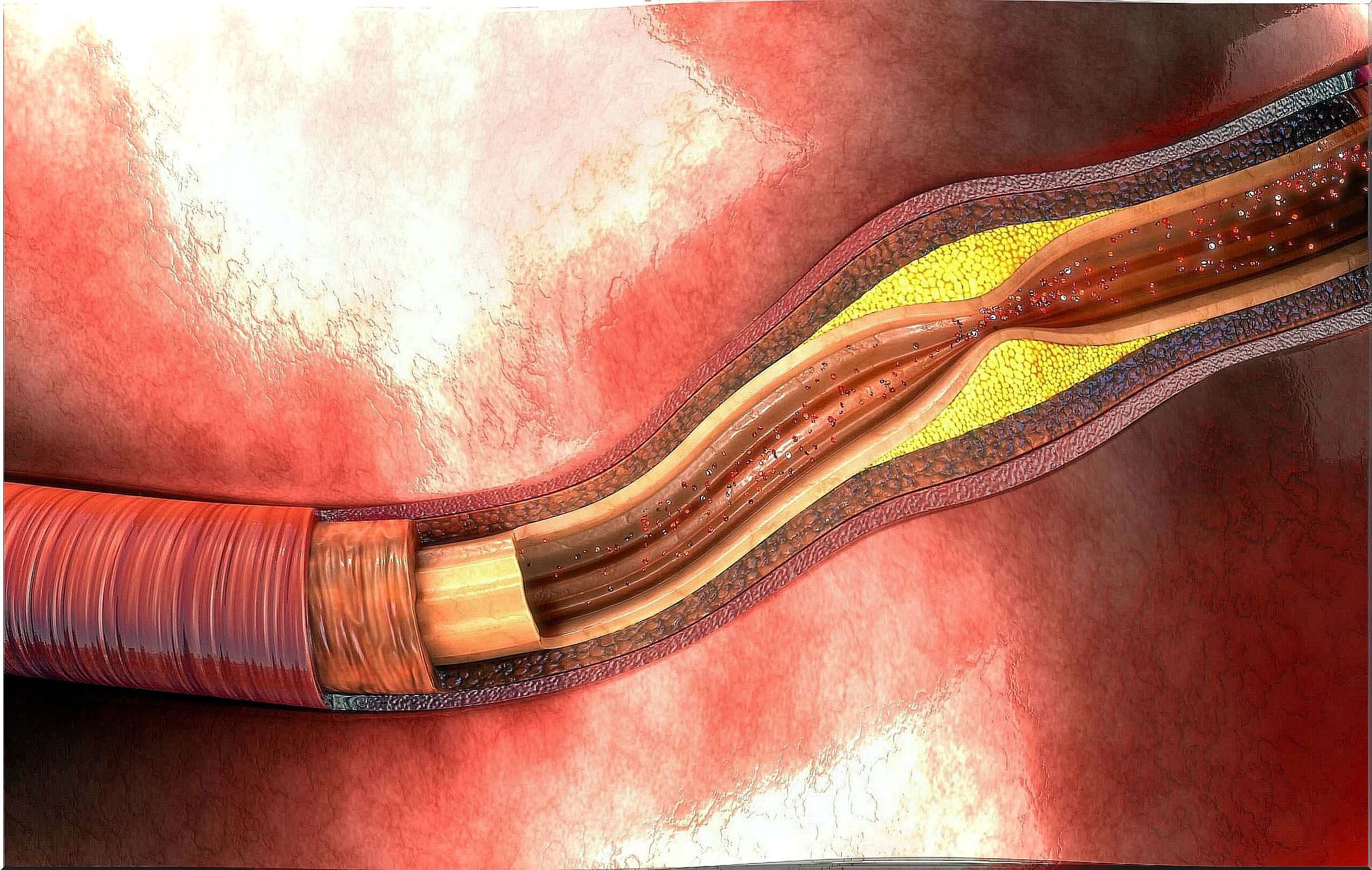
By definition, we speak of peripheral arterial disease when the body’s blood vessels narrow. That is, when they shrink the size of their inner lumen, reducing the flow of blood that can pass through them.
Think of blood vessels as blood transport tubes. These tubes have a certain caliber, that is, a certain interior light that constitutes their diameter. If that diameter decreases, then there is peripheral arterial disease.
Generalities
To be more specific, we have to clarify that this pathology is diagnosed when the affected blood vessels are the large arteries of the human body that are not found in the heart, the aorta system or the brain. Mainly, the arteries involved are those of the limbs.
Whether the origin comes from atherosclerosis, thrombus formation or inflammatory processes, the end result is always the same. The effect of arterial obstruction is the generation of ischemia, this is the lack of blood supply to a part of the body.
Regarding the distribution of peripheral arterial disease, we know that it affects approximately twelve percent of the population. The older the prevalence is, reaching up to twenty percent in people over seventy years of age.
Unfortunately many patients can be asymptomatic. Up to 80% of those who suffer from it find out when it is too late and irreversible damage has already been installed. Therefore, it is important that both patients and doctors learn to know and recognize it.
Causes of peripheral arterial disease
The main and par excellence cause of peripheral arterial disease is atherosclerosis. It is the formation of fatty plaques on the walls of the arteries, which reduces their internal diameter, allowing less blood flow.
The most common place of appearance of these plates are the legs. By decreasing the blood supply in the lower limbs, characteristic symptoms of the pathology that we will name later develop. If it evolves without treatment, the tissues can die from a lack of oxygen and nutrients.
Risk factors have been identified that, being present in the person, increase the possibility of forming atherosclerosis. These factors are as follows:
- Diabetes.
- Smoking
- Aging.
- Arterial hypertension.
- High cholesterol levels.
There is also a substance that scientific studies link to peripheral arterial disease: homocysteine. It is a part of the proteins that participates in different metabolic processes.
Homocysteine would cause failures in the function of the inner layer of the arteries, preventing it from protecting itself from circulating cholesterol. Because of this, the formation of fatty plaques and the risk of creating clots, which are also capable of interrupting blood flow, would increase.
Symptoms
The classic sign of peripheral arterial disease, long described by doctors, is intermittent claudication. It is the appearance of pain when walking, located in the calf, which forces us to stop walking. The pain goes away when you rest.
If the pathology evolves, the pain ceases to be only with exertion and appears at rest. It is a serious sign of progression of the disease. It can appear even at night, interrupting sleep and forcing the patient to wake up.
Other symptoms of the disease are as follows:
- Heaviness in the legs: feeling of fatigue in the muscles of the limbs.
- Weak pulse: in the lower limbs especially.
- Wounds and ulcers of the skin: progressive onset, but slow to heal.
- Skin color changes: Legs may turn pale or bluish.
- Cooling down: one leg colder than the other, for example.
- Poor appendage growth: Toenails or leg hairs can become brittle and grow slowly.
- Erectile dysfunction: Males may have difficulty achieving or maintaining an erection.
Treatment of peripheral vascular disease

There are three approaches to treating peripheral vascular disease: lifestyle changes, medication, and surgery. Sometimes just changing habits is enough, other times medication needs to be added, and in severe cases surgery may be required.
Lifestyle modifications involve quitting smoking if you are a smoker. It is the main measure. Physical activity and a varied and healthy diet are the ideal complement. For those with high blood pressure or diabetes, the recommendations for those diseases apply.
Regarding medications, the treating professional may indicate to the patient drugs that prevent the formation of blood clots, such as aspirin. Cilostazol and pentoxifylline are also used, whose function is to improve blood flow, especially when there is already the symptom of intermittent claudication.
Finally, the last option is surgery. It is reserved for severe cases and consists of three techniques that the professional will choose according to the clinical picture:
- Angioplasty: A catheter is inserted into the affected artery to inflate a balloon there that reopens the blocked area.
- Bypass: a graft is used with a blood vessel from another part of the body or with artificial tissue so that the blood bypasses the obstruction through a kind of bridge.
- Thrombolytic: a drug is injected directly into the artery that is used to dissolve clots.
A complex but treatable disease
Peripheral arterial disease starts when the body’s blood vessels narrow due to the formation of fatty plaques on the arterial walls. Although at first it occurs asymptomatically, over time it can cause serious health complications. Therefore, it is important to receive prompt diagnosis and treatment.